The meniscus, a wedge-shaped piece of cartilage, acts as a “shock absorber” in the knee. Each year, 1.5 million people have surgery to treat meniscus tears in the U.S. and Europe. The people most affected are athletes and the elderly.
Although the most common surgeries, which remove or repair the torn meniscus, can relieve symptoms temporarily, meniscus transplantation is still the best long-term option. However, like other tissue/organ transplantations, this treatment includes many fundamental limitations such as a shortage of donors and the risk of disease transmission. Moreover, managing the supply chain of the transplantation system, which involves meniscus allocation, procurement, testing and transportation, is difficult.
Meniscus and blood vessels are not simple, but they are possible to fabricate, rather than entire organs which are too complex to manufacture using existing technology.
The Solution
Dr. Li Zeng, an assistant professor in the Department of Industrial and Systems Engineering at Texas A&M University, recently received an Operations Engineering Award from the National Science Foundation for her 3D printing-enabled meniscus transplantation system research project. The research project began in 2016 and will be completed in 2019.
Why 3D Printing?
Zeng’s new system will give doctors the ability to create a meniscus substitute, or artificial meniscus, tailored to the characteristics of each patient. “Meniscus and blood vessels are not simple,” said Zeng, “but they are possible to fabricate, rather than entire organs which are too complex to manufacture using existing technology.”
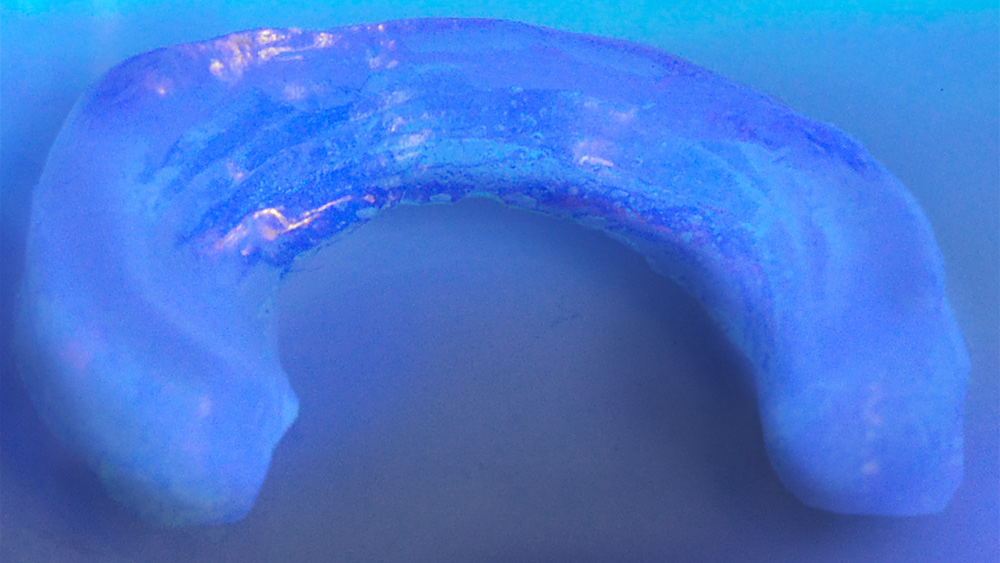
To create the meniscus substitute, a computerized tomography scan or magnetic resonance image of the patient’s knee joint will be input to create the computer-aided design file. Then, the patient’s biological data will be input to create the functional requirements of the meniscus, such as the material and printing conditions. A biomaterial hydrogel will be used to print the scaffold of the meniscus. Cells taken from the patient’s body will fill the scaffold, forming a new tissue and meniscus for the patient. Using the patient’s cells will prevent rejection from the body.
The use of 3D printing will substantially reduce the waiting time for a new meniscus because the system can be placed within the transplantation center to enable doctors to print the artificial meniscus on-site, which means the treatment can be performed immediately. Additionally, fitting problems will no longer occur because the meniscus will be specifically designed and manufactured for the patient. “Ultimately it will change the current donor-based supply chain to an on-demand, personalized paradigm to deliver truly just-in-time, agile and patient-centered care,” said Zeng.
The project is a collaborative study that includes three Texas A&M researchers who are in the fields of in system informatics, manufacturing and biomedical engineering. Zeng, who is the principal investigator, will use the data to find the desired process parameters to create a satisfying product and optimize the overall process. Co-principal investigator Dr. Shiren Wang, associate professor in the industrial and systems engineering department, is an expert on manufacturing and is head of the material design and 3D printing portion of the study. Another co-principal investigator is Dr. Daniel Alge, professor in the Department of Biomedical Engineering, whose specialty is biocompatibility and will focus on the end of the study, ensuring the manufactured meniscus will be accepted by the human body.
Zeng’s research addresses challenges in turning the printer-based meniscus transplantation system into reality, including cost-risk analysis to facilitate decision making, system control for quality assurance and system evaluation for personalized printing.
“For any scientific development,” said Zeng, “you find something promising, then collect data to understand the system and learn how to improve. Data can be very useful to any innovation process.”