A team of researchers at Texas A&M University has developed an innovative way to print therapeutics in 3D for regenerative medicine.
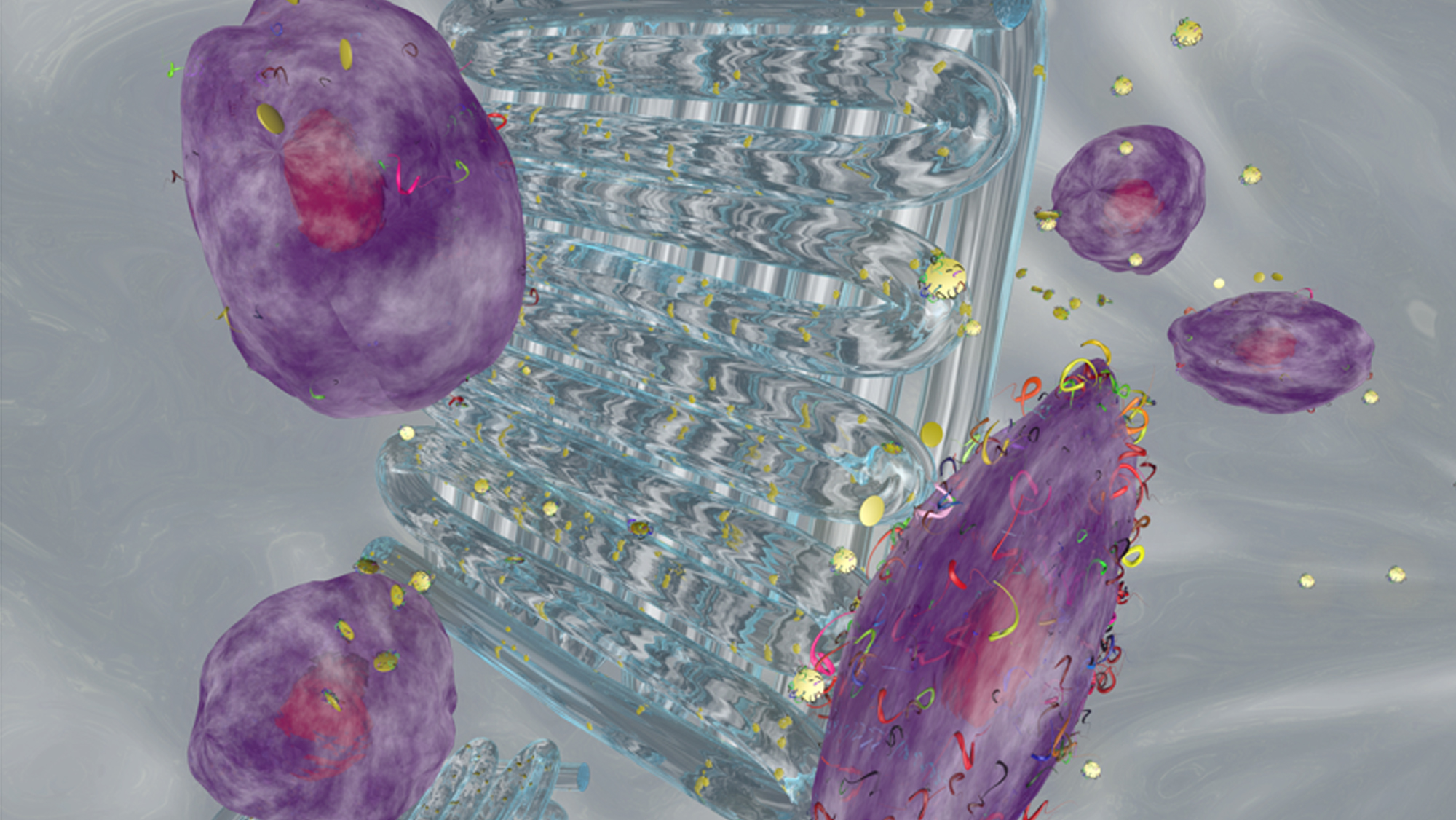
3D bioprinting is emerging as a promising method for rapidly fabricating cell-containing constructs for designing new, healthy, functional tissues. However, one of the major challenges in 3D bioprinting is lack of control over cellular functions. Growth factors, which are a special class of proteins, can direct cellular fate and functions. However, these growth factors cannot be easily incorporated within a 3D-printed structure for a prolonged duration.
In a recent study conducted at Texas A&M, researchers in Dr. Akhilesh K. Gaharwar’s lab in the Department of Biomedical Engineering formulated a bioink consisting of 2D mineral nanoparticles to sequester and 3D print therapeutics at precise locations. Their findings were published in Advanced Healthcare Materials.
The team has designed a new class of hydrogel bioinks — 3D structures that can absorb and retain considerable amounts of water — loaded with therapeutic proteins. This bioink is made from an inert polymer — polyethylene glycol (PEG), and is advantageous for tissue engineering because it does not provoke the immune system. However, due to low viscosity of the PEG polymer solution, it is difficult to 3D print this type of polymer. To overcome this limitation, the team has found that combining PEG polymers with nanoparticles leads to an interesting class of bioink hydrogels that can support cell growth and may have enhanced printability compared to polymer hydrogels by themselves.
This new technology, based on a nanoclay platform developed by Gaharwar, assistant professor, can be used for precise deposition of protein therapeutics. This bioink formulation has unique shear-thinning properties that allow the material to be injected, quickly stop flowing and then cure to stay in place, which is highly desirable for 3D bioprinting applications.
“This formulation using nanoclay sequesters the therapeutic of interest for increased cell activity and proliferation,” said Dr. Charles W. Peak, senior author on the study. “In addition, the prolonged delivery of the bioactive therapeutic could improve cell migration within 3D printed scaffolds and can help in rapid vascularization of scaffolds.”
Gaharwar said the prolonged delivery of the therapeutic could also reduce overall costs by decreasing the therapeutic concentration as well as minimizing the negative side effects associated with supraphysiological doses.
“Overall, this study provides proof of principle to print protein therapeutics in 3D that can be used to control and direct cell functions,” he said.
The research was supported by the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health and the National Science Foundation.