
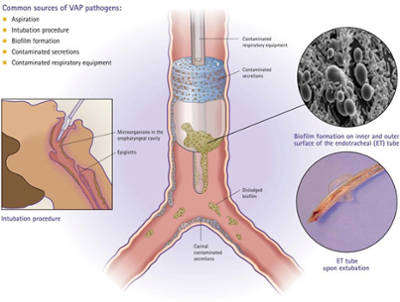
Hospital-acquired infections are a global health problem that threatens patients’ treatment in intensive care units. Patients who require intubation are at a higher risk of contracting life-threatening cases of ventilator-associated pneumonia. Dr. Vanderlei Bagnato, a Hagler Faculty Fellow with the Department of Biomedical Engineering at Texas A&M University, is testing a new cleaning method that may stop these bacteria from spreading.
Bagnato’s work, based out of his lab in Brazil, is focused on using the power of light to destroy bacteria living on the endotracheal tube (ETT), a medical device placed in the patient’s trachea to assist breathing and deliver oxygen into the lungs.
Bagnato said that while the trachea tends to be filled with different bacteria that an individual breathes in, these microorganisms can be attacked by the body’s immune system.
“When people are intubated, very often they do develop pneumonia because that strange surface has no contact with the body’s circulation, so your body cannot fight it,” Bagnato said. “The immune system cannot get to it. That’s why it’s dangerous. The doctor has to come with very strong antibiotics which fight an infection.”
There’s also concern that aggressive use of antibiotics will lead to more antibiotic-resistant bacteria, also referred to as “superbugs.”
As a physicist, Bagnato, professor in the Department of Physics and Materials Science at the University of São Paulo in Brazil, works with light as a physical element. One common technique he uses is photodynamic inactivation, where certain molecules are exposed to light and produce a free radical oxygen molecule, which is destructive.
Placing these molecules in the body can help with a variety of treatments, including cancerous tumors.
“The same thing happens to the microorganism,” Bagnato said. “If I put a molecule and the microorganism close together, that molecule, in the presence of light, will produce the reactive oxygen and then destroy the bacteria.”
The aim of Bagnato’s work is to prevent the progression of an infection as soon as possible after a patient is intubated.
“I consider this a very nice addition to the present technology of artificial breathing because infection developed in the mechanical ventilators is a problem,” Bagnato said.
Bagnato’s team has identified the molecule that works best against the microorganisms on the tubes, a challenge that involved making sure the identified molecule would harm the bacteria without negatively impacting the patient. The molecule sticks to the tube, and then a one-millimeter fiber optic is fed into the tube to light and activate the molecule.
“It’s a low intensity,” Bagnato said. “This means that if we prevent infection, we give a better chance to the patient who is already on the mechanical ventilator.”
Bagnato’s team is now using an artificial trachea to evaluate how long the antimicrobial effect lasts, since these tubes typically remained placed in a patient’s trachea for days.
“I hope that in six, seven months, we’re going to do the first clinical trial,” Bagnato said.